Introduction
See Contents
The healthcare payer solutions market is seeing strong expansion, propelled by changes in healthcare environments and advancements in technology. According to a recent report, by Mordor Intelligence, the market was valued at USD 66.85 billion in 2023 and is poised to reach USD 123.74 billion by 2031, growing at an annual growth rate (CAGR) of 8.0% from 2024 to 2031. This expansion is propelled by several key factors reshaping the industry.
Drivers of Growth
One of the primary drivers accelerating the healthcare payer solutions market is the surge in health insurance enrollments worldwide. As more individuals and organizations embrace health insurance, the demand for efficient payer solutions intensifies, fostering market expansion.
Moreover, technological advancements play a pivotal role in transforming the landscape. Innovations such as AI-driven analytics and interoperable systems enhance operational efficiency and affordability. These advancements benefit healthcare payers by streamlining processes and improving patient outcomes through more effective healthcare delivery.
Dominance of Third-Party Solutions
Third-party vendors dominate the healthcare payer solutions market, offering cost-effective and scalable solutions catering to diverse payer needs. Third-party solutions are favored for their affordability compared to in-house custom developments and their ability to scale effectively across organizations of varying sizes. Furthermore, these vendors bring deep industry expertise, ensuring compliance with stringent regulations and delivering tailored solutions that meet evolving market demands.
While third-party solutions prevail, there remains a niche for custom solutions, particularly among large payers with unique operational requirements. In such cases, custom solutions offer tailored functionalities that align precisely with specific organizational needs, providing a competitive edge in the market.
Major vendors offer extensive service portfolios, leveraging economies of scale to deliver robust, end-to-end solutions that optimize payer efficiency and enhance service delivery. Let’s look at the major vendors of Healthcare Payer Solutions.
Top Healthcare Payer Solutions
Healthcare payer solutions are essential for managing the complex operations of insurance companies, health plans, and other payer organizations. They streamline processes, ensure compliance, improve patient care, and reduce costs. Here, we explore some of the leading healthcare payer solutions that are transforming the industry.
1. Optum
Optum, a subsidiary of UnitedHealth Group, offers comprehensive payer solutions, including data analytics, claims management, and care management systems. Their tools help improve operational efficiency, reduce costs, and enhance patient care.
- Solutions: Claims management, care management, analytics, pharmacy care services.
- Integration: Through APIs and interoperable data frameworks, enabling smooth data exchange across healthcare networks.
2. Cognizant TriZetto Healthcare Products
Cognizant’s TriZetto suite provides a range of software products designed to streamline healthcare payer operations. Key solutions include claims processing, care management, and network management. TriZetto is known for its scalability and ability to integrate with other systems.
- Solutions: IT services, consulting, digital transformation, and operations management.
- Integration: Using BPM and RPA tools for automating processes, and ensuring interoperability with existing systems.
3. Change Healthcare
Change Healthcare offers a broad array of solutions, including revenue cycle management, payment accuracy, and network solutions. Their technology helps payers improve efficiency, reduce fraud, and ensure compliance with regulatory requirements.
- Solutions: Payment accuracy, revenue cycle management, data analytics, network solutions.
- Integration: Using standardized data formats and APIs for real-time data exchange and automation.
4. Oracle Health Insurance
Oracle Health Insurance provides advanced payer solutions that focus on claims processing, policy administration, and billing. Oracle’s robust data management and analytics capabilities help payers optimize their operations and improve decision-making.
- Solutions: Comprehensive insurance management including claims processing, policy administration, and billing.
- Integration: Via robust APIs, cloud services, and enterprise integration frameworks to connect with existing systems.
5. IBM Watson Health
IBM Watson Health leverages artificial intelligence and machine learning to offer payer solutions that enhance decision-making and operational efficiency. Key services encompass population health management, analytics for value-based care, and fraud detection.
- Solutions: Data analytics, AI-driven insights, care management, and population health management.
- Integration: Using AI and machine learning models, along with standardized data formats and APIs to integrate seamlessly with other healthcare systems.
6. Epic Tapestry
Epic’s Tapestry is specifically tailored for healthcare payers and managed care organizations. It offers comprehensive features for member management, claims processing, and care management. Tapestry is known for its integration with Epic’s electronic health record (EHR) system, providing a seamless experience for users.
- Solutions: Managed care administration, including membership management, claims processing, and provider network management.
- Integration: Through Epic’s extensive interoperability capabilities and APIs that ensure connectivity with other healthcare systems and databases.
7. McKesson Health Solutions
McKesson offers a range of payer solutions, including claims management, payment automation, and decision management systems. Their solutions help payers reduce administrative costs and improve accuracy and compliance.
- Solutions: Revenue cycle management, claims management, and clinical data integration.
- Integration: Employing cloud-based platforms and interoperability standards to integrate with various healthcare systems.
8. Infosys McCamish
Infosys McCamish provides a suite of solutions for healthcare payers, including policy administration, claims processing, and customer service management. Their technology helps payers streamline operations and improve customer satisfaction.
- Solutions: Insurance and healthcare services including policy administration, claims processing, and business process outsourcing.
- Integration: Through scalable IT solutions, APIs, and secure data exchange protocols to facilitate integration with payer systems.
9. HealthEdge
HealthEdge provides HealthRules, a next-generation software platform for healthcare payers. It includes claims processing, care management, and payment solutions, all designed to support value-based care and improve operational efficiency.
- Solutions: Core administration solutions, including claims processing, benefit management, and member engagement.
- Integration: Using a modular platform with open APIs to ensure flexibility and interoperability with other systems.
10. EXL Healthcare
EXL Healthcare offers payer solutions focused on data analytics, care management, and revenue cycle optimization. Their tools help payers improve member outcomes, reduce costs, and enhance operational efficiency.
- Solutions: Data analytics, care management, and revenue cycle management.
- Integration: Leveraging advanced analytics platforms and interoperability frameworks to integrate data from various sources.
How Healthcare Payer Solutions Work?
Healthcare payer solutions aim to enhance operational efficiency and effectiveness for insurance companies, health plans, and other payer organizations. According to a report from Grandview Research, the North America healthcare payer services market was valued at USD 47.0 billion in 2022 and is projected to grow at a CAGR of 7.3% over the forecast period. The increasing demand for healthcare IT services is expected to fuel the growth of the healthcare supply chain business process outsourcing market during this period.
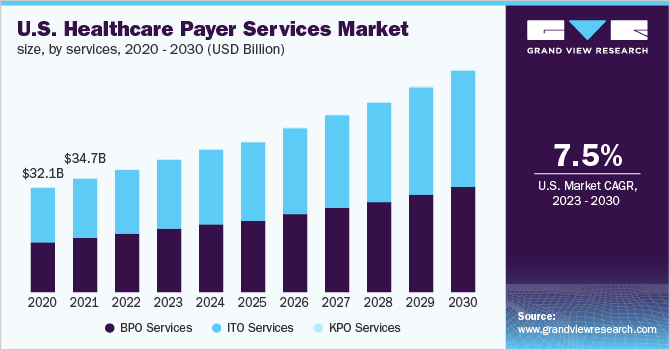
Changes in regulatory landscapes and mounting pressure on the healthcare industry to reduce service costs are expected to boost further the demand for healthcare supply chain business process outsourcing. As a result, significant growth is forecasted for the regional market over the coming years.
Benefits of Healthcare Payer Solutions
- Efficiency: Automation reduces administrative burdens and speeds up processes.
- Cost Savings: Identifying and eliminating inefficiencies and fraud reduces costs.
- Improved Outcomes: Enhanced care coordination and management lead to better patient outcomes.
- Compliance: Healthcare payer solutions ensure compliance with regulatory requirements and industry standards.
- Member Satisfaction: Providing timely information and support improves member experience.
Healthcare payer solutions integrate advanced technologies and data-driven approaches to streamline operations, enhance care management, and improve overall efficiency and patient outcomes within the healthcare system.
What is the cost of integration?
The cost of integrating healthcare payer solutions varies widely, typically from $500,000 to several million dollars. This includes expenses for software licensing, implementation, data migration, customization, training, and ongoing support. Pricing varies based on factors such as the complexity of existing systems, the scope of healthcare payer solutions, and the level of customization needed. Investing in healthcare payer solutions integration can yield substantial long-term savings and operational efficiencies.
Integrating healthcare payer solutions involves significant costs, primarily driven by several key factors:
- Software Licensing: Acquiring licenses for core administration systems, analytics platforms, and other specialized software components can be expensive, depending on the vendor and solution complexity.
- Implementation Services: Costs associated with planning, configuring, and deploying the integrated solutions across the organization. This includes project management, system configuration, and initial setup.
- Data Migration: Moving data from legacy systems to the new integrated platform requires careful planning and execution. Costs include data cleansing, transformation, and ensuring data integrity during the migration process.
- Customization: Tailoring the healthcare payer solutions to meet specific organizational needs and workflows often involves additional development costs. This may include customizing interfaces, and reports, and integrating with existing IT infrastructure.
- Training and Change Management: Providing training sessions for staff to familiarize them with new systems and processes. Change management efforts to facilitate the smooth adoption of new technologies also add to the overall cost.
- Support and Maintenance: Ongoing support services, including help desk support, software updates, and system maintenance, are essential for ensuring the continued operation and optimization of integrated healthcare payer solutions.
- Infrastructure and IT Costs: Investment in hardware infrastructure, cloud services, and IT resources necessary to support integrated solutions and ensure scalability and reliability.
- Compliance and Security: Costs associated with implementing and maintaining regulatory compliance measures such as HIPAA, GDPR, and cybersecurity protocols to protect sensitive healthcare data.
- Consulting and Integration Services: Engaging consultants and integration specialists to design, integrate, and optimize healthcare payer solutions, ensuring they meet organizational goals and industry standards.
The overall cost of integrating healthcare payer solutions can vary widely based on the project’s scope and complexity. Organizations should carefully assess their needs, budget constraints, and expected return on investment to justify the expenditure and maximize the benefits of streamlined operations and improved healthcare service delivery.
Conclusion
In conclusion, the trajectory of the healthcare payer solutions market is defined by dynamic growth fueled by expanding health insurance enrollments and transformative technological innovations. While third-party vendors dominate with scalable, cost-effective solutions tailored to industry standards and regulations, custom solutions, exemplified by providers like Emorphis Health, cater to specific organizational needs with bespoke functionalities.
Emorphis Health stands out for its expertise in integrating both custom and third-party solutions seamlessly, ensuring comprehensive healthcare integration services. This strategic approach not only enhances operational efficiency but also reinforces the industry’s commitment to delivering superior patient care and navigating evolving regulatory landscapes effectively. As the market continues to evolve, the synergy between custom solutions and third-party integrations will remain pivotal in shaping the future of healthcare payer solutions.