Overview
See Contents
When navigating the world of digital healthcare, one common debate is EHR vs. EMR. Because both terms are often used interchangeably, it’s crucial to understand the differences. This distinction holds significance not just for healthcare providers but also for patients who are increasingly active in managing their healthcare journey. Moreover, the choice between EHR vs. EMR impacts how health information is managed and shared.
What is an EMR?
An Electronic Medical Record (EMR) represents a digital version of a patient’s chart. Because it is primarily used by healthcare providers, it contains the medical and treatment history of patients within one practice. Furthermore, EMRs are a great improvement over paper records. They help in tracking data over time, identifying patients due for preventive visits, and monitoring patient progress. However, EMRs are limited in that they are designed for use within one facility and don’t easily share information with other healthcare systems.
What is an EHR?
An Electronic Health Record (EHR), on the other hand, is a more comprehensive digital record of patient health. Also, unlike EMRs, EHRs are designed to be shared across different healthcare settings. Because they include information from all the clinicians involved in a patient’s care, EHRs provide a broader view of a patient’s health. Moreover, EHRs can be accessed by various healthcare providers, such as specialists, pharmacies, and labs, making them a more versatile tool in healthcare management.
The Electronic Health Records (EHR) and Electronic Medical Records (EMR) market is substantial and continues to grow significantly. In 2023, the global EHR-EMR market was valued at around USD 30.4 billion, with a forecasted Compound Annual Growth Rate (CAGR) of 6.21% from 2024 to 2032. The market is dominated by key players such as GE Healthcare, Cerner Corporation, and Allscripts, with North America holding the largest market share due to the high adoption rate of these systems in the region.
Europe is the second-largest market, driven by technological advancements and increasing government support. Meanwhile, the Asia-Pacific region is expected to witness the highest growth, primarily due to the rising awareness and government initiatives in countries like China, Japan, and India.
For more detailed insights, refer to the Market Research Future report and Mordor Intelligence report for more detailed insights.
Now, let us check the major differences between EHR vs EMR.
Key Differences: EHR vs. EMR
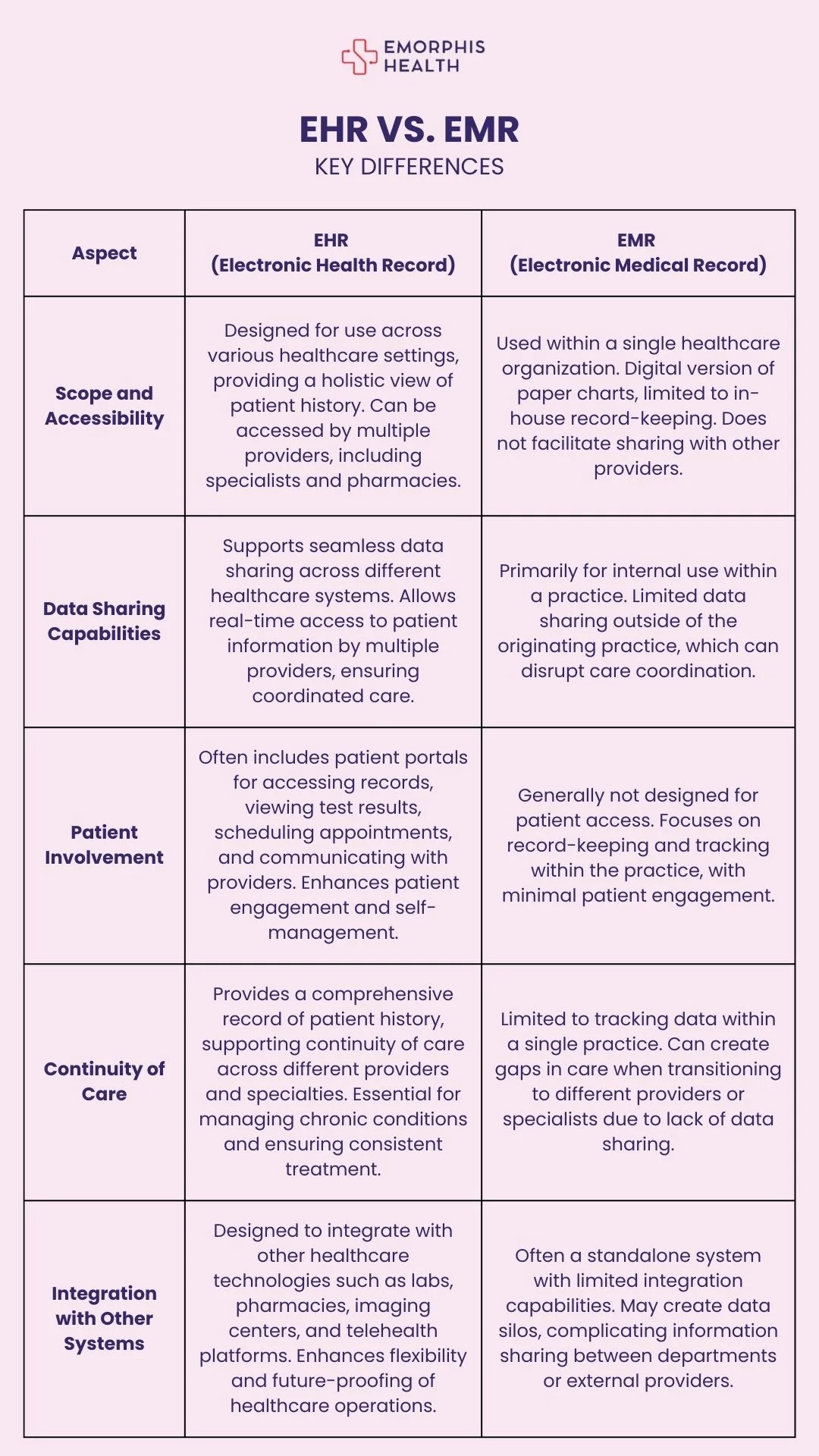
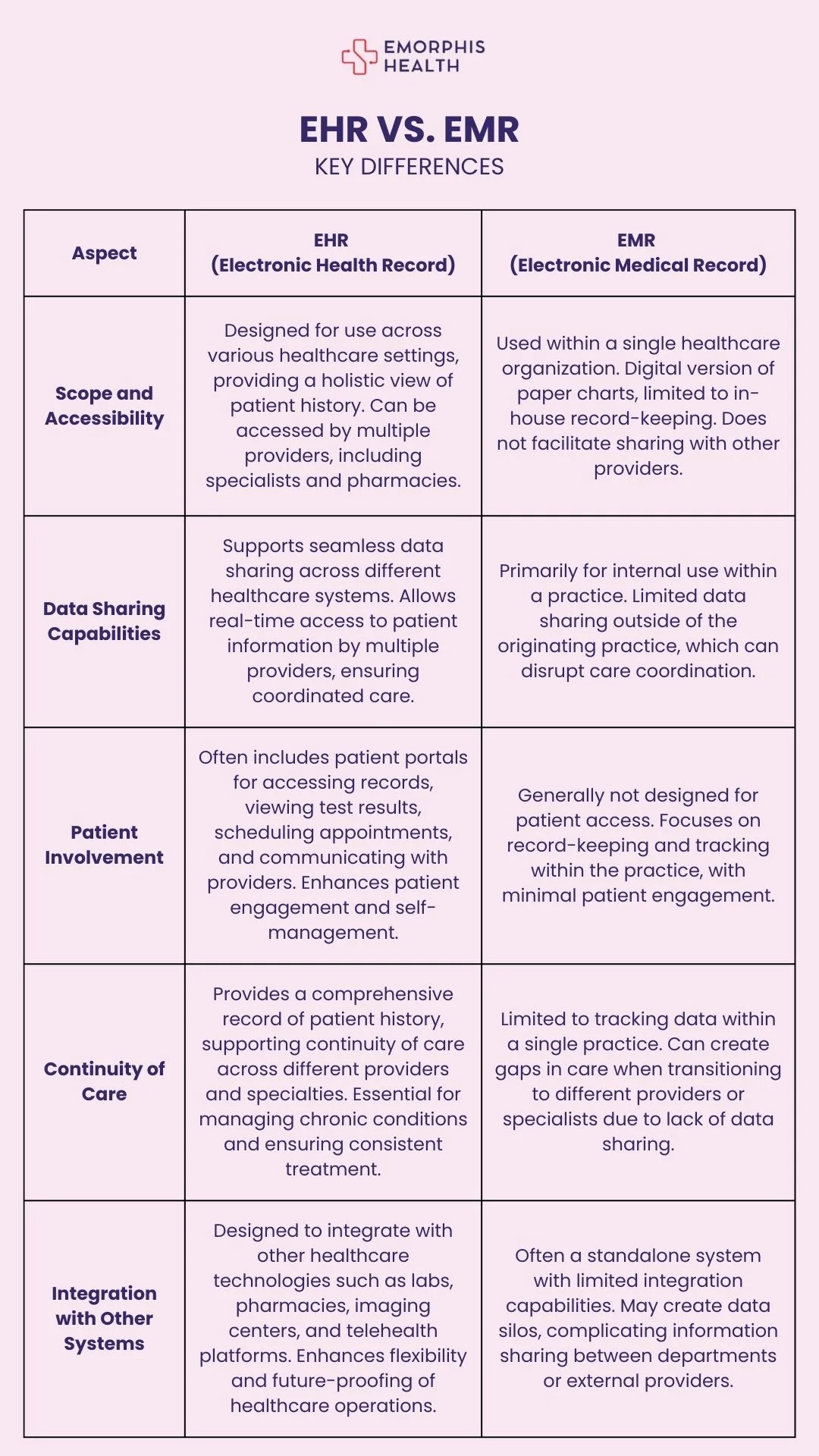
When comparing EHR vs. EMR, it’s essential to understand the fundamental differences that set them apart. Because these differences impact how health data is utilized, they play a critical role in patient care and healthcare operations. Moreover, each system serves distinct purposes within the healthcare industry, making it important to know which is more suitable for specific needs. Let’s break down the key differences between EHR vs. EMR into several important aspects.
1. Scope and Accessibility
One of the primary differences between EHR vs. EMR lies in their scope and accessibility. EMRs are designed to be used within a single healthcare organization, which means they are essentially digital versions of paper charts used for in-house record-keeping. Because EMRs are confined to one practice, they don’t facilitate easy sharing of information with other healthcare providers.
EHRs, on the other hand, are designed with interoperability in mind. Moreover, they are meant to be shared across different healthcare settings, providing a more holistic view of a patient’s medical history. Also, EHRs can be accessed by multiple healthcare providers, including specialists, labs, and pharmacies, which makes them far more versatile. Furthermore, this broader scope makes EHRs a critical tool in ensuring continuity of care.
2. Data Sharing Capabilities
Another key difference in the EHR vs. EMR comparison is their ability to share data. EMRs are primarily used for internal use within a healthcare practice. Because of this, they do not easily support data sharing outside of the originating practice. Moreover, the lack of data-sharing capabilities in EMRs can lead to challenges in coordinating care, especially when patients need to see multiple providers.
In contrast, EHRs are specifically designed to share data seamlessly across different healthcare systems. Also, EHRs allow for real-time sharing of patient information among various healthcare providers, ensuring that everyone involved in a patient’s care has access to the same up-to-date information. Furthermore, this capability is particularly important in modern healthcare, where coordinated care across various specialties is often necessary.
3. Patient Involvement
When considering EHR vs. EMR, it’s important to note how each system impacts patient involvement. EMRs are typically used by healthcare providers for record-keeping and tracking patient information within the practice. Because EMRs are not designed to be accessed by patients, they do not offer much in terms of patient engagement or self-management.
However, EHRs offer a different approach. Moreover, EHRs often come with patient portals that allow individuals to access their health records, view test results, schedule appointments, and communicate with their healthcare providers. Also, this level of access empowers patients to take a more active role in their healthcare, making them partners in their care journey. Furthermore, patient involvement is increasingly recognized as a key factor in achieving better health outcomes, which is why EHRs are becoming the preferred choice for many healthcare organizations.
4. Continuity of Care
The ability to provide continuous care is another significant difference in the EHR vs. EMR debate. EMRs are limited to tracking patient data within a single practice, which can create gaps in care when a patient transitions to a different provider or requires care from multiple specialists. Because EMRs do not offer easy data sharing, continuity of care can be disrupted, leading to potential errors and inefficiencies.
EHRs, however, are designed to ensure continuity of care. Moreover, they provide a comprehensive record that follows the patient throughout their healthcare journey, regardless of where they receive care. Also, EHRs allow healthcare providers to see the full picture of a patient’s health history, which leads to more informed decision-making and better-coordinated care. Furthermore, this continuity is crucial in managing chronic conditions, where consistent monitoring and treatment adjustments are often necessary.
5. Integration with Other Systems
Integration capabilities are another area where EHR vs. EMR differ significantly. EMRs are often standalone systems that do not easily integrate with other healthcare technologies. Because of this, they can create data silos, making it difficult to share information between different departments or external healthcare providers.
In contrast, EHRs are designed with integration in mind. Moreover, EHRs can easily connect with other healthcare systems, such as laboratories, pharmacies, and imaging centers, to provide a more comprehensive view of a patient’s health. Also, EHRs often integrate with other digital tools, such as telehealth platforms and wearable devices, to enhance patient care. Furthermore, this ability to integrate with various systems makes EHRs a more flexible and future-proof solution for healthcare organizations.
Here is the difference between EHR and EMR in an image format.
Conclusion: Choosing Between EHR vs. EMR
In summary, the key differences between EHR vs. EMR highlight the importance of choosing the right system for your healthcare needs. Because EMRs are more limited in scope and data-sharing capabilities, they are often better suited for smaller practices with less need for external communication. Also, they provide a straightforward way to digitize paper records without requiring extensive changes to existing workflows.
However, EHRs offer a more comprehensive and integrated approach, making them ideal for larger healthcare organizations or those that require coordinated care across multiple providers. Moreover, the ability to share data, involve patients and ensure continuity of care makes EHRs a more powerful tool in modern healthcare. Furthermore, as healthcare continues to evolve, EHRs are likely to play an increasingly central role in improving patient outcomes and streamlining healthcare delivery.
Connecting with Emorphis Health experts for EHR integration services ensures you’re tapping into a reservoir of specialized knowledge and experience. Our team excels in navigating the complexities of EHR systems, seamlessly integrating them into your existing infrastructure to enhance efficiency and patient care. By choosing Emorphis, you benefit from a tailored approach that considers your unique needs, ensuring a smooth transition and robust system performance.
Our experts provide end-to-end support, from initial consultation to implementation and ongoing optimization, making EHR integration services, a streamlined and hassle-free experience. Let Emorphis guide you toward a more connected and efficient healthcare environment.