The integration of Electronic Health Records (EHRs) is a critical component of modern healthcare IT systems. Whether you are developing a telehealth platform, patient engagement solution, or healthcare analytics tool, seamless EHR integration is essential for interoperability, compliance, and efficiency. Two common approaches exist; let’s look at EHR aggregators vs custom integration. Using an EHR aggregator or opting for custom EHR integration.
Let us explore both options, weighing their benefits, drawbacks, and ideal use.
Understanding EHR Aggregators
See Contents
- 1 Understanding EHR Aggregators
- 2 Trending EHR Aggregators
- 3 Understanding Custom EHR Integration
- 4 EHR Aggregators vs Custom Integration: Key Differences
- 5 EHR Aggregator vs. Custom Integration: When to Choose What?
- 6 What You Need in Custom EHR Integration?
- 7 Is Custom EHR Integration Right for You?
- 8 Final Thoughts
EHR aggregators are third-party platforms that provide a single API to connect with multiple EHR systems like Epic, Cerner, Meditech, and Athenahealth. Instead of developing separate integrations for each EHR provider, organizations can leverage aggregators to streamline access to patient records, appointment scheduling, and clinical data exchange.
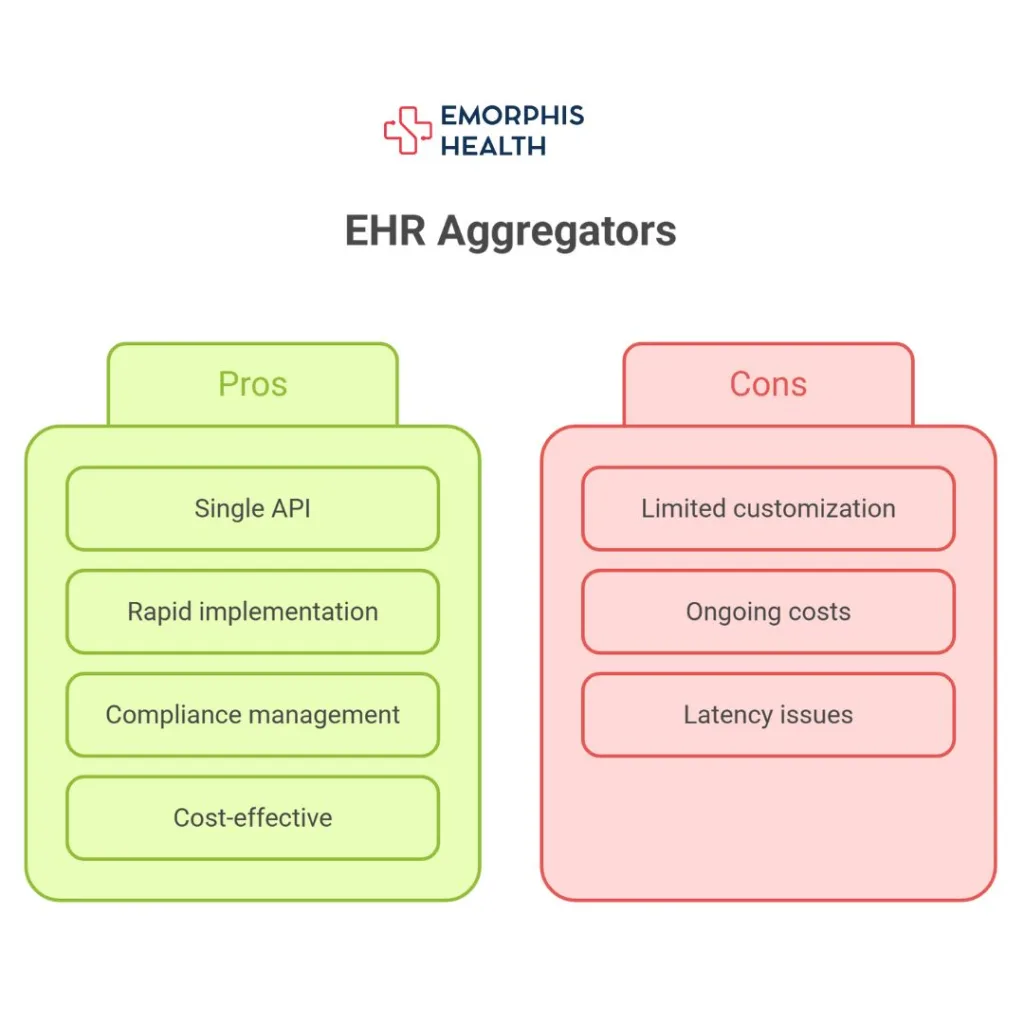
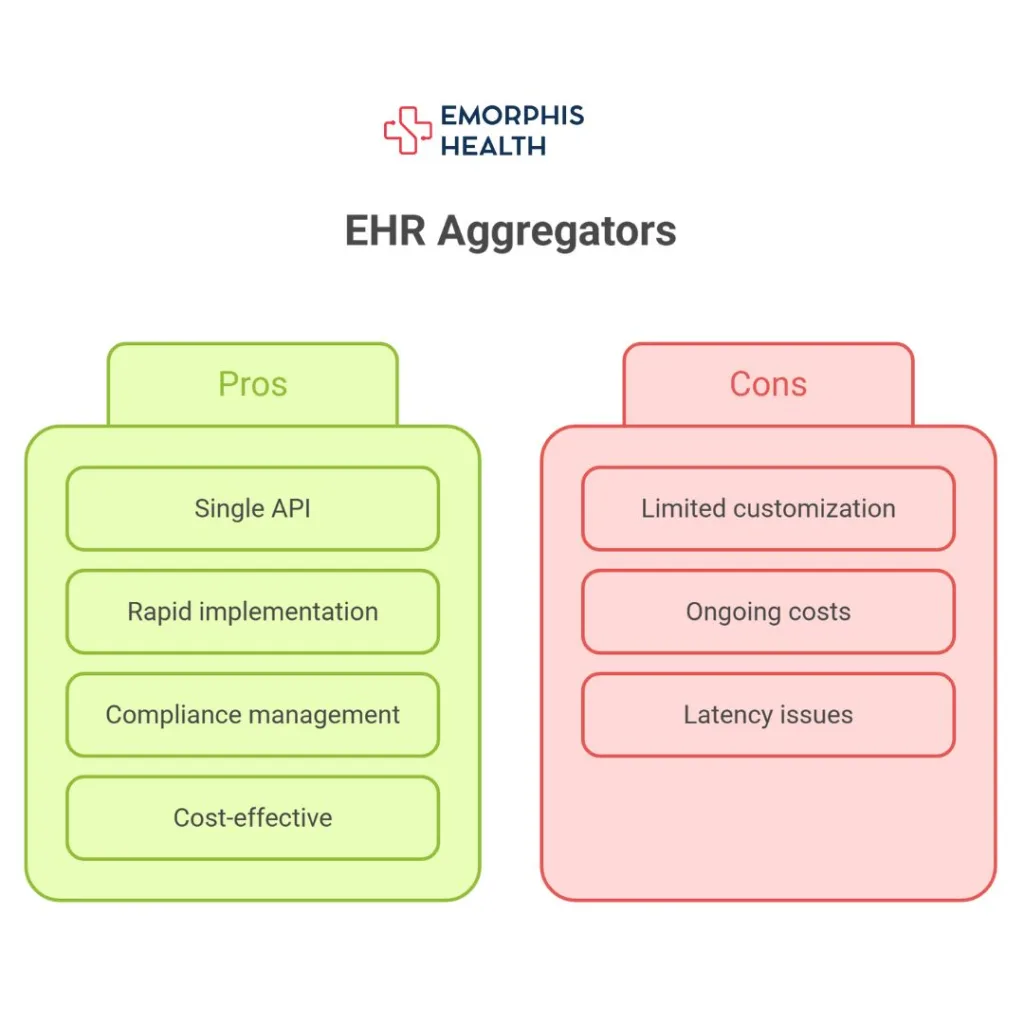
Pros of EHR Aggregators
One of the biggest advantages of using an EHR aggregator is the ability to access multiple EHR systems through a single API. This eliminates the need to build and maintain separate integrations for each vendor, significantly simplifying the process for healthcare technology companies. With a single point of connection, organizations can quickly access patient records, appointment scheduling, and other critical healthcare data without the hassle of managing multiple interfaces.
Another major benefit of EHR aggregators is the speed of implementation. Since they provide a pre-built solution that already connects to multiple EHR vendors, healthcare organizations can quickly integrate with different systems without having to spend months or even years developing custom integrations. This rapid deployment is particularly beneficial for startups or companies looking to launch new healthcare applications quickly.
EHR aggregators also manage ongoing compliance with healthcare regulations, such as HIPAA, ONC, and other relevant industry standards. This means that organizations using an aggregator do not have to worry about keeping up with constantly evolving compliance requirements, as the aggregator ensures adherence to necessary regulations.
Additionally, for startups and small businesses, EHR aggregators offer a cost-effective solution. Instead of investing heavily in a dedicated development team to build and maintain direct integrations with multiple EHRs, companies can simply use an aggregator’s service at a fraction of the cost.
Cons of EHR Aggregators
Despite their many advantages, EHR aggregators come with some limitations. One of the main drawbacks is the restricted level of customization. Because organizations must rely on the aggregator’s API, they are limited to the functionalities and data access provided by the third-party service. If a company requires advanced workflows or specialized data fields, an aggregator may not be the best choice.
Another downside is the ongoing cost. While aggregators help reduce initial development expenses, they typically operate on a subscription or transaction-based pricing model. Over time, these recurring costs can add up, potentially making the solution more expensive in the long run compared to a custom-built integration.
Lastly, because an EHR aggregator acts as an intermediary, there can be latency issues when retrieving data. Since data must first pass through the aggregator before reaching the end user, the speed of data exchange may not be as fast as a direct connection with an EHR system.
Lets look at some of the trending EHR Aggregators
Trending EHR Aggregators
| Aggregator | Overview / Strengths |
| Redox | One of the most established aggregators; supports FHIR, HL7, and proprietary EHR APIs. Trusted by major digital health players. |
| Particle Health | Focuses on real-time clinical data exchange with national networks like Carequality and CommonWell. |
| Ellkay | A long-standing healthcare data aggregator specializing in interoperability. Offers connectivity with 600+ EHR, practice management, and laboratory systems. Provides APIs, HL7, CCD, and flat file integration, making it a strong choice for digital health apps needing broad connectivity across legacy and modern systems. |
| Tangible | Focuses on simplifying healthcare data exchange with FHIR-first APIs. Provides developer-friendly infrastructure for accessing EHR data securely and efficiently. Known for fast implementation and scalable integration, it caters to digital health startups and enterprises looking to accelerate time-to-market with interoperable solutions. |
| Health Gorilla | Offers full clinical data interoperability, lab networks, and national exchange access. Also a TEFCA QHIN. |
| 1upHealth | Built on FHIR-first principles; supports large-scale population health and payer-provider integration. |
| Zus Health | Developer-friendly aggregator that unifies patient data and offers tools for building digital health products. |
| Bridge Connector | Focuses on workflow automation and EHR integration without needing custom code. |
| Medplum | Open-source healthcare API platform offering FHIR-native aggregation and analytics-ready architecture. |
| Validic | Specializes in remote patient monitoring and integrates wearable/device data with EHRs. |
| Healthjump | Offers structured clinical data extraction and normalization from EHRs. |
| Human API | Aggregates real-time consumer health data (including EHR, labs, wearable) for insurers, researchers, and digital health apps. |
Notable Mentions:
- Komodo Health – While not a pure EHR aggregator, it provides access to a massive healthcare data ecosystem with real-world evidence and claims data.
- Cloudticity – Focuses on compliance-first healthcare cloud infrastructure with data aggregation for analytics.
- Datavant – Known for privacy-preserving health data exchange, often combined with EHR integration for research and analytics.
Understanding Custom EHR Integration
Custom EHR integration involves directly connecting a healthcare application to one or multiple EHRs using vendor-specific APIs or interoperability standards such as HL7 and FHIR. This approach provides complete control over data exchange, allowing for a tailored integration that meets specific business and clinical needs.
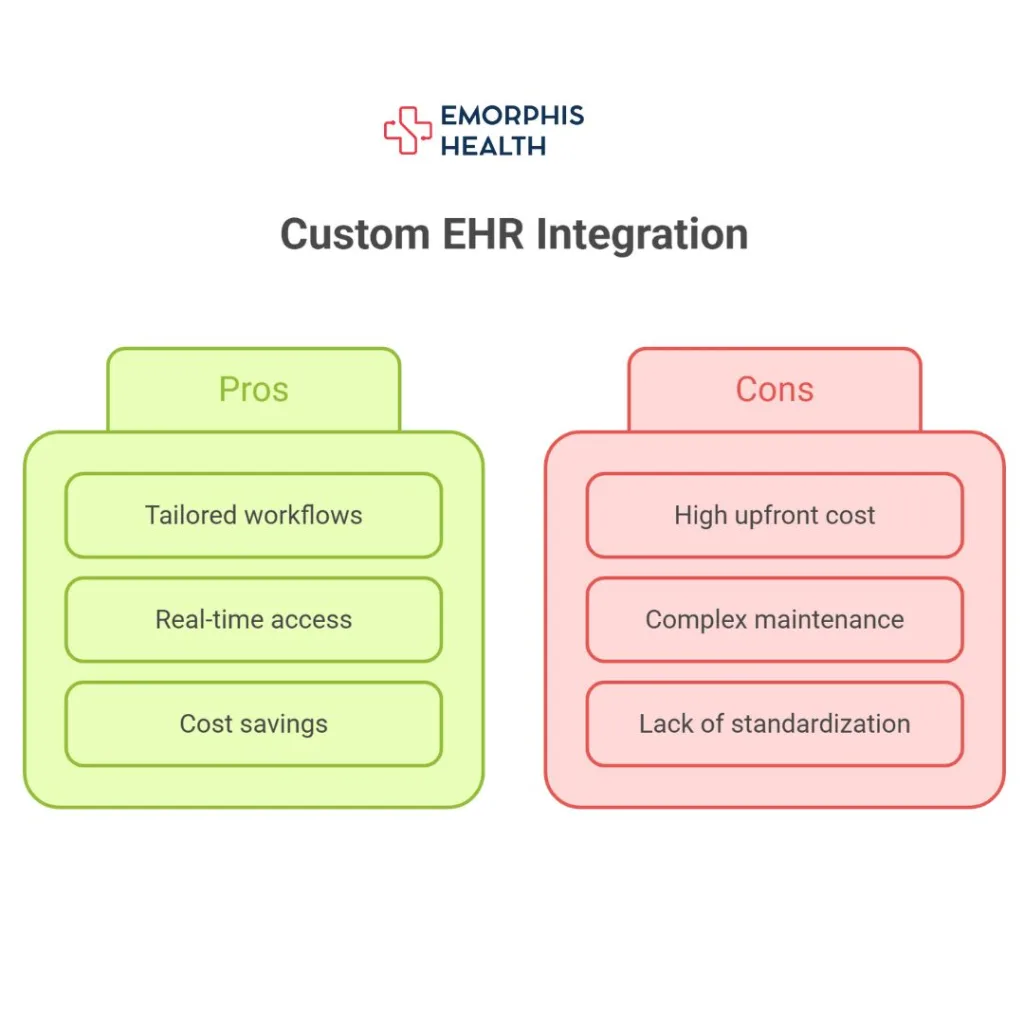
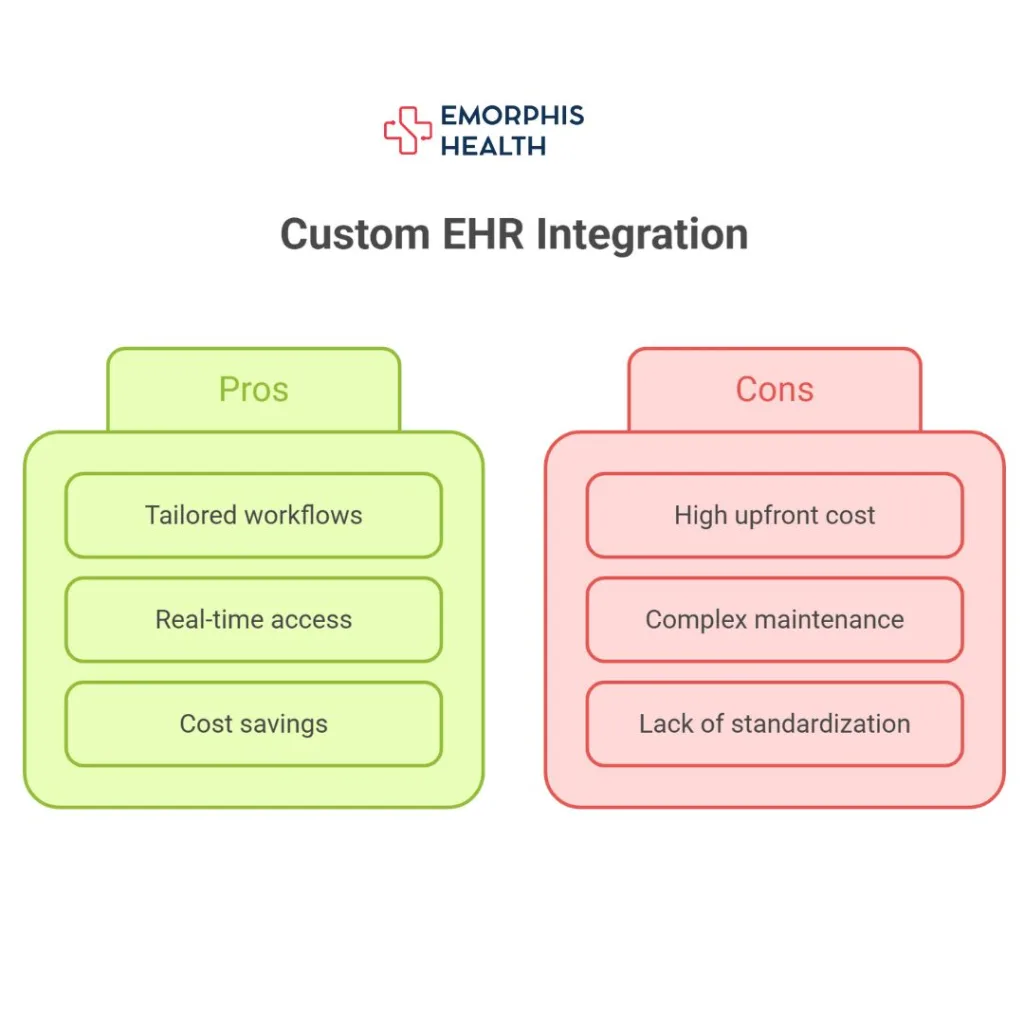
Pros of Custom EHR Integration
One of the biggest advantages of custom integration is the ability to tailor the solution to specific requirements. Organizations can design workflows that precisely fit their operational needs, ensuring that data is exchanged in the most efficient and meaningful way possible. This level of customization is particularly important for healthcare providers with complex processes that require advanced interoperability features.
Custom integration also enables direct access to EHR data, ensuring real-time speed and efficiency. Unlike an aggregator, which may introduce latency due to its intermediary role, a direct connection allows organizations to retrieve and process data without any delays. This is especially critical for real-time applications, such as telemedicine platforms or clinical decision support systems.
Another long-term benefit of custom integration is cost efficiency. While the initial development cost may be high, organizations can avoid the ongoing subscription or transaction fees associated with aggregators. Over time, this can lead to significant cost savings, especially for larger healthcare organizations with high data transaction volumes.
Cons of Custom EHR Integration
Despite its advantages, custom integration comes with challenges. One of the main barriers is the high upfront cost and complexity. Unlike using an aggregator, which simplifies the process, custom integration requires significant development resources and expertise. Organizations need a skilled development team familiar with EHR APIs, HL7, FHIR, and other healthcare interoperability standards.
Ongoing maintenance is another consideration. When an EHR provider updates its API or makes changes to compliance requirements, organizations with custom integrations must manage these updates internally. This requires dedicated IT resources to ensure that the system remains operational and compliant with regulations.
Additionally, integrating with multiple EHR systems can be challenging due to the lack of standardized APIs across vendors. Each EHR provider may have its own proprietary data structures and authentication methods, making it complex to establish and maintain multiple connections. This is a major hurdle for organizations looking to scale across various healthcare networks.
Lets now check the differences with a table.
EHR Aggregators vs Custom Integration: Key Differences
| Feature / Aspect | EHR Aggregator | Custom Integration |
|---|---|---|
| Definition | A third-party platform that connects to multiple EHR systems via standardized APIs | Directly building and managing integrations between your system and each EHR |
| Integration Model | Plug-and-play; unified API across multiple EHRs | One-to-one integration with each EHR system |
| Speed to Deploy | Fast; can be deployed in days or weeks | Slow; requires weeks to months per integration |
| Development Effort | Minimal; integration logic is abstracted | High; must handle individual EHR quirks and standards manually |
| Technical Maintenance | Managed by aggregator vendor | Your team handles all versioning and updates |
| Interoperability Standards | FHIR, HL7, C-CDA (standardized across EHRs via aggregator) | FHIR, HL7, C-CDA (must implement per EHR vendor specifications) |
| Data Normalization | Automatically normalized across systems | Must manually normalize formats from different EHRs |
| Customization Flexibility | Limited to the aggregator’s supported schema and endpoints | Fully customizable to your specific data and logic needs |
| Vendor Lock-In | Yes; you’re dependent on the aggregator for connectivity and updates | No; you control all code, connectors, and logic |
| Compliance & Security | Aggregator handles HIPAA, SOC2, and audit logging | You must ensure compliance and maintain security protocols |
| Cost | Subscription-based; can be expensive at scale or per-record | Higher upfront development cost but potentially lower long-term recurring cost |
| Scalability | Easily scalable to more EHRs and data types through aggregator | Scalability is resource-intensive and adds complexity per EHR added |
| Support for Rare EHRs | Limited to aggregator’s existing integrations | Possible if your team builds custom connectors |
| Real-Time Data Access | May offer batch or delayed sync (depends on aggregator) | Can be built for true real-time exchange |
| Control Over Data Flow | Limited visibility and control over internal workings | Full control and transparency |
| Use Cases | Ideal for startups, pilot projects, MVPs, and broad data access across systems | Best for enterprise-level solutions needing custom workflows or deep EHR integration |
| Example Vendors / Tools | Redox, Health Gorilla, Particle Health, Zus Health, 1upHealth | Direct FHIR/HL7 integrations with Epic, Cerner, Allscripts, etc. |
| Onboarding New EHRs | Fast, if supported by aggregator | Slow and manual; each EHR needs unique integration |
| Reliability | Dependent on aggregator uptime | Your team is responsible for reliability and error handling |
| Analytics & Reporting | Some aggregators offer built-in analytics | Must be built separately |
| Future-Proofing | May lag in supporting new EHR features or regulations | Can immediately adapt to changes if you have the resources |
EHR Aggregator vs. Custom Integration: When to Choose What?
For startups and companies looking to deploy their healthcare applications quickly, an EHR aggregator is often the best choice. It provides an easy, cost-effective way to connect with multiple EHR systems without requiring extensive development work. Companies focused on rapid market entry and minimal maintenance should consider this option.
On the other hand, custom EHR integration is ideal for organizations that need deep customization, direct control over data exchange, and long-term cost savings. Established healthcare providers, enterprise applications, and businesses that require highly specific workflows should invest in a tailored integration solution to ensure seamless interoperability.
Let’s now walk through everything you need to build a robust, secure, and scalable custom EHR integration, from technical components to compliance requirements and beyond.
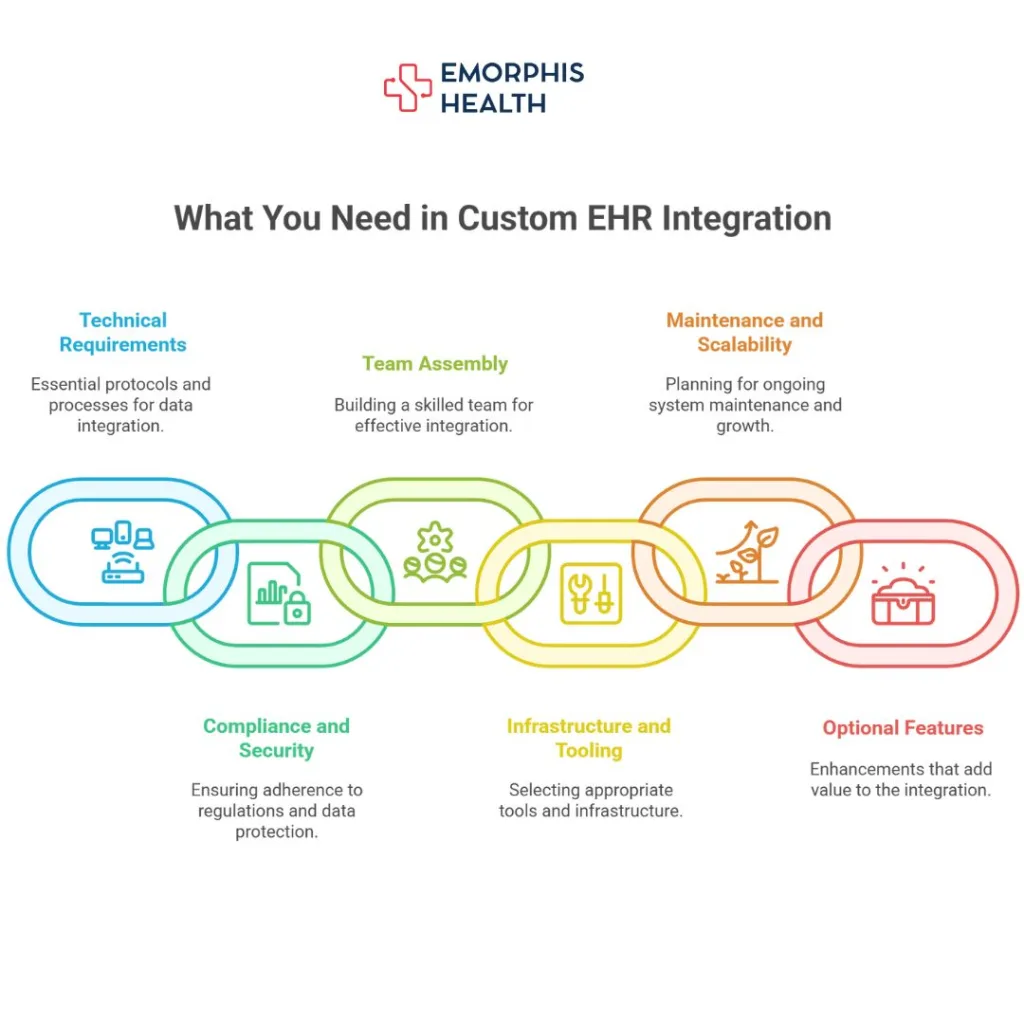
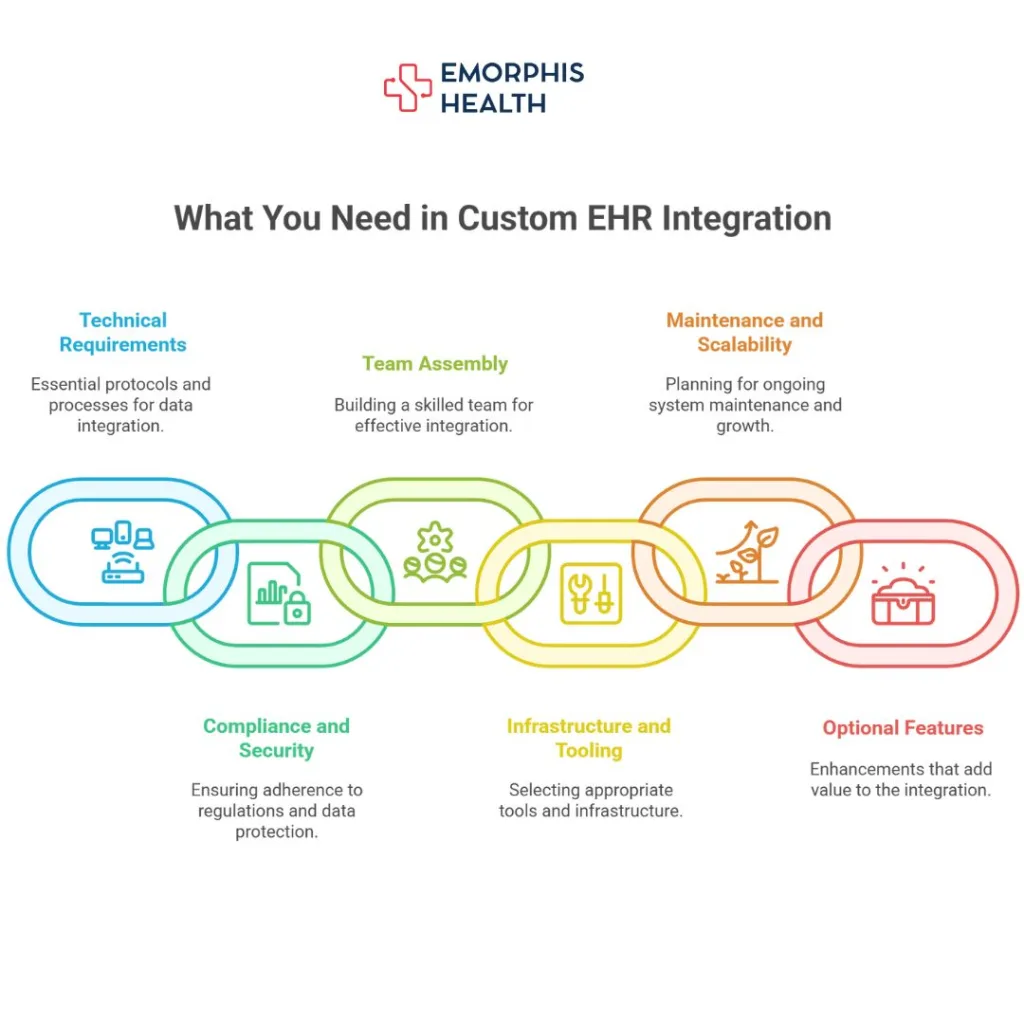
What You Need in Custom EHR Integration?
1. Define Your Integration Strategy
The first step in custom EHR integration is to clearly define why you’re integrating and what outcomes you’re trying to achieve. This involves:
- Identifying the EHR systems involved (e.g., Epic, Cerner, Athenahealth, eClinicalWorks).
- Choosing the data types you need: patient demographics, lab results, medications, appointments, encounters, notes, etc.
- Determining the direction of data flow: whether it’s a read-only sync, a write-back feature, or full bidirectional integration.
- Selecting integration types: modern APIs like FHIR, older HL7 v2 messages, C-CDA documents, or even direct database/file-based methods.
The goal here is to build a roadmap so your technical, compliance, and business teams align from day one.
2. Core Technical Requirements
Once your strategy is clear, the next step is building the technical foundation. A successful custom EHR integration requires the following components:
a) FHIR and HL7 Protocol Support
- Use FHIR APIs for modern EHRs (structured, RESTful access).
- Support HL7 v2.x messaging for legacy systems.
- Parse C-CDA documents when structured documents are provided.
- Implement schema mapping logic to handle variation across vendors.
b) Data Normalization
- Standardize incoming data to a common internal schema.
- Handle inconsistent data formats across EHRs.
- Ensure compatibility for downstream apps or analytics engines.
c) Authentication and Authorization
- Implement OAuth 2.0 or SMART on FHIR for secure access.
- Use API keys or tokens for EHRs with custom auth.
- Include token refresh and revocation handling.
- Enforce role-based permissions and scopes.
d) Middleware or ETL Pipelines
- Build ETL layers to extract, transform, and load clinical data.
- Transform vendor-specific formats to your internal models.
- Route data intelligently based on source and purpose.
- Modularize for scalability and easier debugging.
e) Error Handling and Logging
- Capture errors in real-time with detailed logs.
- Implement retry logic for failed transmissions.
- Create dashboards or alerts for integration failures.
- Maintain audit logs for compliance and debugging.
f) Queue Management
- Use Kafka, RabbitMQ, or similar tools for async data flow.
- Ensure decoupled, fault-tolerant architecture.
- Improve throughput and system reliability during spikes.
- Prioritize critical messages in processing queues.
3. Compliance and Security Essentials
Healthcare data integration is subject to stringent regulatory standards. Custom EHR integration must ensure HIPAA compliance and robust data security:
- HIPAA Compliance: All handling of Protected Health Information (PHI) must follow HIPAA guidelines including access control, breach notification, audit trails, and encryption.
- Encryption: Use TLS/SSL for data in transit and AES-256 or better for data at rest.
- Access Control: Role-based access and granular permission models should be enforced for internal teams and external APIs.
- Audit Trails: Track who accessed what, when, and why—down to the API level.
- Business Associate Agreements (BAAs): If integrating with other third-party vendors or providers, ensure you have appropriate BAAs signed.
Security isn’t optional; it must be embedded at every layer of your system.
4. Assembling the Right Team
Custom integrations are technically demanding. You’ll need a team with the following roles and responsibilities:
- Solution Architect: Designs the system architecture and ensures scalable design.
- Integration Developers: Skilled in FHIR, HL7, C-CDA, and data transformation.
- Security & Compliance Officer: Oversees all regulatory and security protocols.
- DevOps Engineer: Manages infrastructure, CI/CD pipelines, monitoring, and deployment.
- QA/Testing Engineers: Ensure all data flows work correctly and data accuracy is maintained.
Without a skilled team, even the best integration plan can fail in execution.
5. Infrastructure and Tooling
Your custom EHR integration requires a solid technical stack and infrastructure for both development and production environments. Consider the following:
- API Gateway (e.g., Kong, Apigee): Manage access, rate limiting, and authentication for APIs.
- Monitoring Tools (e.g., Datadog, Prometheus, ELK Stack): Track system health, performance, and errors.
- Data Storage: Use a compliant and secure database or data lake to store normalized EHR data.
- CI/CD Pipelines: Automate code testing, deployment, and updates to ensure seamless releases.
- Version Control: Git-based source control for managing changes to APIs, configurations, and integration logic.
6. Maintenance and Scalability Planning
Integration is not a one-time effort. You must plan for ongoing maintenance, monitoring, and scaling:
- EHR API Version Updates: EHR vendors frequently update their APIs. Track these changes and update your integration logic accordingly.
- Data Accuracy Audits: Regularly verify that the data retrieved or written is correct and complete.
- Error Resolution: Build dashboards or alerting systems to track and fix failed syncs or API issues.
- User Feedback Channels: Allow clinicians, admins, or app users to report integration bugs quickly.
- Documentation: Maintain updated technical documentation, API specs, and user guides for internal and external stakeholders.
If your platform expands to support multiple EHRs or new workflows, scalability planning becomes critical.
7. Optional but Valuable Features
To enhance your integration and future-proof it, consider implementing these:
- SMART on FHIR App Integration: Allows apps to launch inside EHR systems with full context (patient ID, encounter ID).
- Consent Management: Build workflows to collect and track patient authorization for data access.
- Custom Dashboards: Visual interfaces for monitoring sync status, errors, data volume, or latency.
- Analytics Integration: Enable downstream applications like dashboards, risk scores, or predictive modeling using the collected data.
These features may not be mandatory at launch, but they add significant long-term value.
Is Custom EHR Integration Right for You?
Custom EHR integration offers maximum control, flexibility, and customization, especially for companies with complex workflows or proprietary data requirements. However, it comes with trade-offs—higher upfront cost, longer development time, and ongoing maintenance responsibilities.
If you’re building an enterprise-grade solution or need deep, reliable, and highly tailored EHR data flows, custom integration is often the best path forward.
But to succeed, you must invest in:
- A clear strategy
- Technical excellence
- Regulatory compliance
- Scalable infrastructure
If you’re unsure whether to go this route or use a third-party aggregator, we can help evaluate both options in detail, tailored to your business model, timeline, and target markets.
Final Thoughts
Both EHR aggregators and custom EHR integration have their advantages and drawbacks. The right choice depends on your organization’s goals, budget, and technical capabilities. While aggregators offer convenience and speed, custom integrations provide full control and scalability. By evaluating the specific needs of your healthcare application, you can determine the best approach for ensuring efficient, secure, and compliant EHR interoperability.
If you need expert assistance in EMR/EHR Development and Integration Services, our team at Emorphis Health specializes in healthcare software development. Contact us to explore the best solutions for your interoperability needs!