Introduction
See Contents
- 1 Introduction
- 2 Why Economics of AI in Healthcare Matters
- 3 The Shifting ROI Models of AI in Healthcare
- 4 Proven Use Cases of Economics of AI in Healthcare
- 5 How Strategies with AI are Driving Economic Value in Healthcare
- 6 ROI Models for AI in Healthcare
- 7 Challenges and Risks in Realizing ROI from AI in Healthcare
- 8 Key Trends Shaping the Future ROI of AI in Healthcare
- 9 Conclusion
Artificial Intelligence is no longer a futuristic concept in healthcare. From predictive diagnostics to personalized treatment plans, AI is already shaping the way providers, payers, and technology companies operate. Yet behind all the excitement lies a serious question: what is the real economic value of AI in healthcare?
Many organizations have tested AI pilots, but few have developed a clear understanding of return on investment (ROI). Without a strong financial case, it is difficult for hospitals, payers, or life sciences companies to scale AI adoption. This is where the economics of AI in healthcare becomes a critical conversation.
Understanding the economics of AI means going beyond technology. It involves measuring cost savings, revenue growth, operational efficiencies, and patient outcomes in a way that is sustainable and measurable. This article will explain ROI models that work, highlight real-world applications, and guide decision-makers on how to approach AI investments strategically.
Why Economics of AI in Healthcare Matters
Healthcare is a sector that operates under constant pressure: rising costs, growing patient expectations, complex regulations, and workforce shortages. Traditional methods of cost optimization have reached their limits. AI provides a new lever, but decision-makers often hesitate due to unclear financial justification.
The economics of AI is not only about technology cost. It is about creating value-based healthcare models where efficiency, outcomes, and patient satisfaction improve at the same time. For example:
- AI-enabled diagnostic systems can detect diseases earlier, reducing expensive late-stage treatments.
- Predictive algorithms can optimize hospital staffing, lowering overtime and burnout-related costs.
- Automation in administrative workflows reduces claims denial rates, improving cash flow for providers.
In each case, the value goes far beyond simple cost-cutting. It reshapes how healthcare systems work financially and operationally.
The Shifting ROI Models of AI in Healthcare
ROI in healthcare AI is different from ROI in other industries. A retail company may measure AI success based on direct revenue growth. In healthcare, ROI often requires balancing financial return with clinical outcomes.
There are several ROI models that organizations use today:
1. Cost Reduction Model
This is the most direct way to measure ROI. It focuses on reducing operational costs through AI adoption. Examples include:
- Automating claims processing with AI, reducing administrative staff time.
- Using AI to optimize medical imaging analysis, cutting radiology turnaround times.
- Streamlining supply chain logistics with predictive AI models to reduce waste.
2. Revenue Enhancement Model
Here, AI generates new revenue opportunities. Examples include:
- AI-driven remote patient monitoring services reimbursed by insurers.
- Personalized patient engagement solutions that increase adherence and retention.
- AI-powered clinical trial optimization that brings new drugs to market faster.
3. Value-Based Care Model
With the shift toward outcome-based reimbursement, AI becomes an enabler of value-based care. ROI is measured by reduced readmissions, improved chronic disease management, and better patient satisfaction scores.
4. Hybrid ROI Model
Most real-world implementations combine cost reduction and value creation. A hospital deploying AI for early sepsis detection reduces ICU costs while also improving survival rates, thus creating a double ROI effect.
Proven Use Cases of Economics of AI in Healthcare
The theory becomes more meaningful when seen in practice. Let us look at some proven use cases where AI has created measurable financial and clinical impact.
-
Radiology Efficiency
Hospitals that use AI in radiology have reported turnaround time reductions of up to 50%. Faster reporting not only improves patient flow but also reduces bottlenecks that often increase costs. -
Predictive Readmission Prevention
AI models can identify high-risk patients who are likely to be readmitted within 30 days. By intervening early with care management, hospitals reduce penalties from insurers and improve patient outcomes. -
Revenue Cycle Automation
Claims denials are a huge cost burden for providers. AI-powered solutions that analyze denial patterns and automate coding have been shown to improve revenue recovery significantly. -
Drug Discovery Acceleration
In life sciences, AI shortens the time needed to identify viable drug candidates. This reduces R&D costs and brings therapies to market faster, improving ROI for pharma companies.
How Strategies with AI are Driving Economic Value in Healthcare
Artificial Intelligence is not just a technology trend in healthcare. It is a force reshaping the economic foundation of hospitals, clinics, insurers, and even medical device makers. The economics of AI in healthcare revolves around the balance between cost savings, efficiency gains, and improved patient outcomes. Let us break this down into measurable areas of impact.
1. Cost Savings Through Automation
AI reduces repetitive manual tasks that consume both time and money. Some clear examples include:
- Administrative efficiency: AI-powered coding and claims processing cut billing errors and speed up reimbursements.
- Clinical documentation: Natural Language Processing (NLP) tools automatically create notes from doctor-patient conversations, reducing physician burnout and saving hours per week.
- Supply chain optimization: Predictive analytics ensures the right amount of medical supplies are stocked, reducing waste.
Each of these areas translates directly into financial savings, often visible within the first year of deployment.
2. Revenue Growth Through Better Patient Engagement
Healthcare is no longer only about treating illness. It is about creating a relationship with patients, improving their experience, and ensuring loyalty. AI helps in this through:
- Personalized patient communication: AI chatbots and virtual assistants guide patients before and after treatments.
- Predictive retention models: Algorithms predict which patients are likely to miss follow-ups or discontinue treatment, helping providers take preventive steps.
- Smarter scheduling: AI tools reduce no-shows by sending reminders and offering flexible rescheduling options.
Better patient engagement not only improves care but also ensures a stable revenue cycle for healthcare providers.
3. Reduced Clinical Errors and Liability Costs
Medical errors are among the costliest challenges in healthcare. AI supports clinicians with:
- Decision support systems that highlight possible risks in diagnosis and treatment.
- Drug interaction checks powered by machine learning.
- Real-time alerts for abnormal patient vitals in hospitals.
The reduction in malpractice risks and penalties has a direct financial benefit, improving overall ROI.
Upgrading Your Health Cloud with AI, choose custom AI Solutions – Read a Practical Guide for CTOs and Product Teams
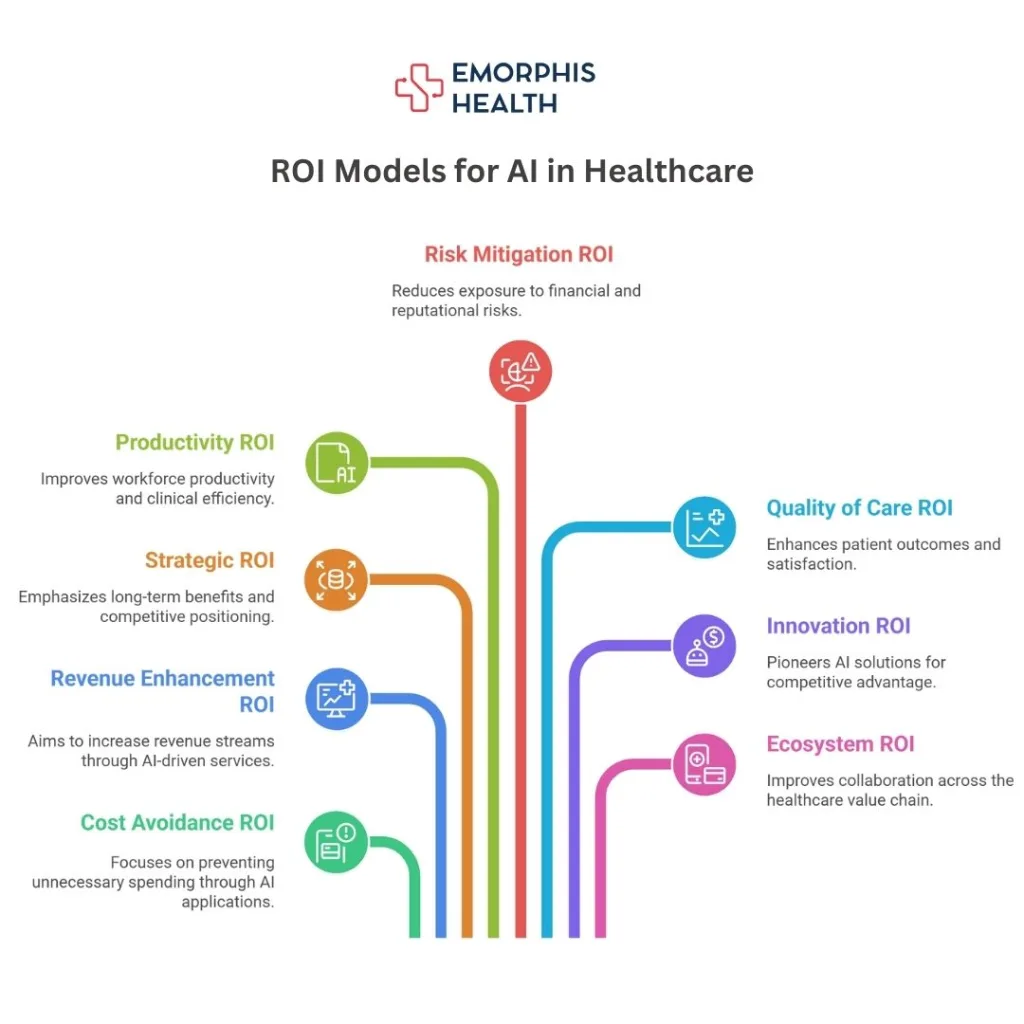
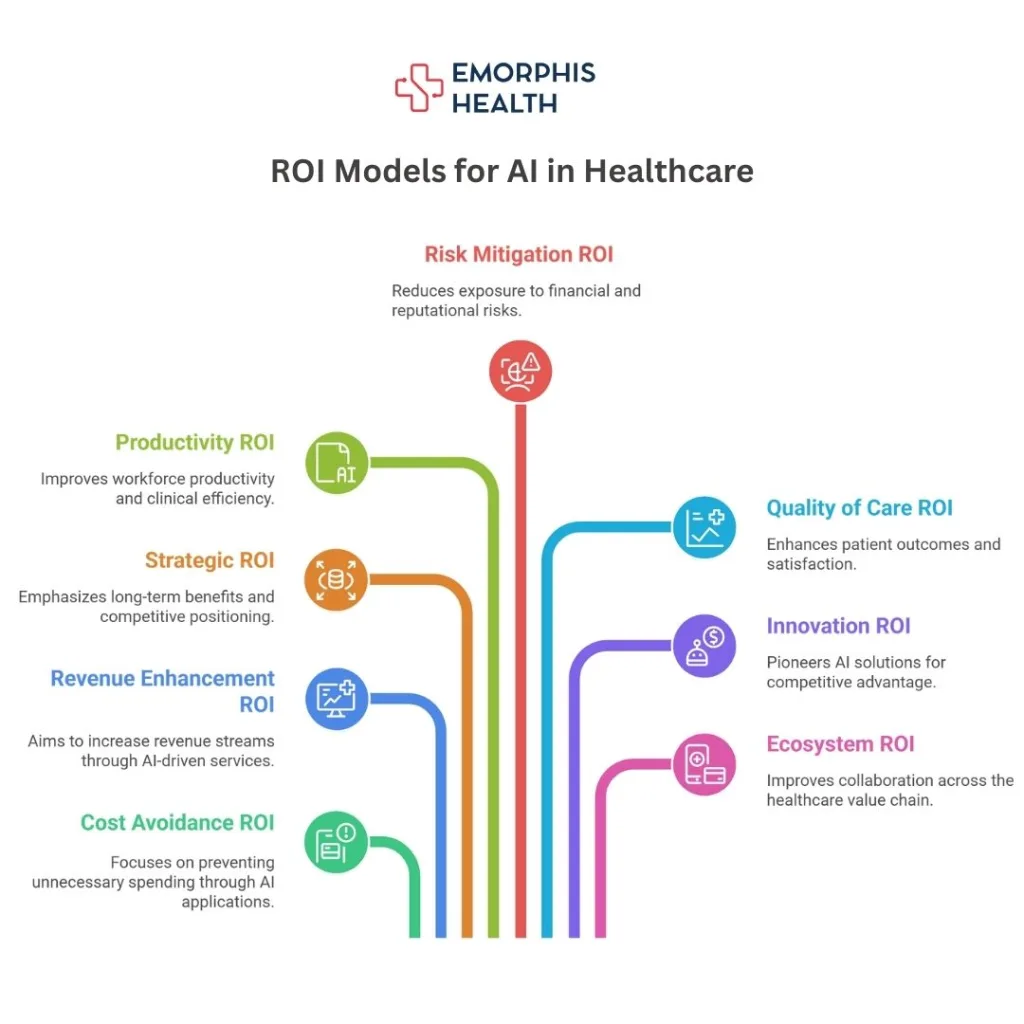
ROI Models for AI in Healthcare
Understanding ROI in AI healthcare projects requires moving beyond simple “cost versus revenue” calculations. The economics of AI in healthcare can be explained through three major ROI models.
Model 1: Cost Avoidance ROI
This model measures how AI prevents unnecessary spending. Examples include:
- Avoiding readmissions through AI-powered monitoring.
- Preventing diagnostic errors that lead to costly re-tests or litigation.
- Reducing manual labor costs in areas such as data entry.
Hospitals that adopt AI for readmission prevention often save millions of dollars annually.
Model 2: Revenue Enhancement ROI
This model calculates how AI actively contributes to new or improved revenue streams. For example:
- AI-driven patient engagement platforms leading to higher patient retention.
- AI-enabled precision medicine services that allow providers to charge premium fees.
- Integration of AI telehealth tools expanding patient reach beyond physical geographies.
Revenue enhancement ROI is particularly relevant for private hospitals and specialty care providers seeking growth.
Model 3: Strategic ROI
This model is more long term. It includes benefits that may not show immediate financial returns but strengthen the organization’s position in the future. Examples include:
- Building a data infrastructure that makes the hospital attractive for research partnerships.
- Leveraging AI insights for population health management, aligning with value-based care models.
- Creating intellectual property through AI-powered innovations in diagnostics or treatment planning.
Strategic ROI ensures that healthcare providers remain competitive in a market increasingly shaped by digital transformation.
Model 4: Productivity ROI
This model focuses on measuring how AI improves workforce productivity and clinical efficiency. It does not only look at reducing costs but also at enabling more value from the same set of resources.
Examples include:
- AI-assisted clinical documentation tools reducing time doctors spend typing notes.
- Automating repetitive administrative workflows such as insurance claims or scheduling.
- Decision-support AI that allows doctors to see more patients in the same amount of time.
By reducing time waste and freeing up skilled resources, hospitals can treat more patients without proportionally increasing staff numbers, which translates directly to better margins.
Model 5: Risk Mitigation ROI
Healthcare is a high-risk industry with compliance, litigation, and patient safety at stake. Risk mitigation ROI measures how AI reduces exposure to financial and reputational risks.
Examples include:
- AI-driven fraud detection in billing and insurance claims.
- Compliance-focused AI ensuring adherence to HIPAA, GDPR, or local regulatory frameworks.
- Predictive analytics for identifying high-risk patients early, reducing the chances of malpractice claims.
This ROI is often hidden until a major compliance fine or lawsuit is avoided. Institutions that proactively invest in AI see long-term savings by minimizing these risks.
Model 6: Quality of Care ROI
This model evaluates the improvement in patient outcomes as a measurable return. While harder to express in dollars, quality of care ROI often translates into revenue and compliance benefits in value-based care systems.
Examples include:
- AI-driven personalized treatment plans improving recovery rates.
- Early disease detection models reducing the need for expensive late-stage interventions.
- Patient satisfaction scores increasing due to shorter wait times and more accurate diagnoses.
Higher care quality leads to improved hospital ratings, greater patient trust, and in some cases, higher reimbursement rates under value-based care models.
Model 7: Innovation ROI
Innovation ROI looks at the financial and reputational benefits of pioneering AI solutions ahead of competitors.
Examples include:
- Hospitals developing proprietary AI algorithms and licensing them to other providers.
- Attracting research grants or partnerships with pharmaceutical companies through AI data infrastructure.
- Positioning as a “digital-first hospital,” drawing patients and talent who prefer technologically advanced institutions.
While not always immediate, innovation ROI is a competitive differentiator that creates new revenue streams and future-proofs the organization.
Model 8: Ecosystem ROI
Ecosystem ROI focuses on how AI adoption improves collaboration across the healthcare value chain, creating financial and strategic advantages.
Examples include:
- AI systems that integrate seamlessly with EHR vendors, labs, and insurers, reducing friction across the ecosystem.
- Enabling interoperability with HL7 and FHIR standards to make the hospital a more attractive partner.
- Strengthening relationships with insurance payers by proving cost-efficiency through AI-supported care delivery.
This model goes beyond internal returns and measures value in terms of broader healthcare partnerships and system-wide trust.
Challenges and Risks in Realizing ROI from AI in Healthcare
While the economics of AI in healthcare is promising, realizing strong ROI is not automatic. Many organizations fail to see expected returns because of avoidable mistakes or overlooked risks.
Common Challenges:
-
Data silos and poor interoperability
Healthcare data often lives in different systems, making integration into AI models difficult. Without proper interoperability frameworks such as HL7 and FHIR, ROI projections can fall short. -
Hidden implementation costs
Beyond licensing or development costs, organizations must budget for training, workflow redesign, infrastructure upgrades, and regulatory compliance. -
Regulatory uncertainty
Compliance with HIPAA, GDPR, FDA guidelines for SaMD, and emerging AI-specific regulations adds complexity. -
Trust and adoption by clinicians
If clinicians do not trust the AI’s recommendations or if workflows are disrupted, adoption slows and expected returns shrink. -
Cybersecurity risks
AI systems managing sensitive health data are prime targets for cyberattacks, making strong security investments a non-negotiable.
How to Overcome These Risks:
- Start with small, high-ROI pilot projects before scaling.
- Ensure strong data governance and interoperability from day one.
- Build multidisciplinary teams including clinicians, IT, and AI specialists.
- Incorporate explainable AI (XAI) to improve trust.
- Partner with experienced AI software development company who understands both healthcare and compliance.
Key Trends Shaping the Future ROI of AI in Healthcare
Looking forward, the economics of AI in healthcare will evolve from experimental investments to measurable, predictable financial models.
1. Value-based care models
As more health systems shift from fee-for-service to value-based care, AI will prove its worth by reducing readmissions, improving population health outcomes, and supporting preventative care—all of which deliver measurable ROI.
2. Integration with digital health ecosystems
AI will not remain a standalone solution. Instead, it will be embedded across EHR systems, telehealth platforms, IoMT devices, and population health dashboards. This interconnectedness will compound ROI across departments.
3. AI-driven drug development economics
The cost of bringing a new drug to market could be reduced by billions through AI-based molecular discovery, patient stratification, and trial design optimization.
4. Scalable infrastructure via cloud AI services
Cloud AI reduces the upfront cost barrier for healthcare organizations. Pay-as-you-go models will make ROI calculations more favorable, especially for smaller hospitals.
Read more details on How to Build Scalable AI-Powered Applications with Cloud AI Services.
5. Shift from cost savings to revenue growth
Initially, AI investments are justified by cost reductions in labor and operations. In the future, revenue generation from AI-powered digital health services, new care delivery models, and partnerships will dominate ROI calculations.
Conclusion
The economics of AI in healthcare is no longer an abstract concept. It is a boardroom discussion, a CIO priority, and a CMO strategy driver. From cost savings to revenue generation, the financial models are clear: AI, when implemented strategically, delivers measurable and repeatable ROI.
However, the journey requires precision. Poor planning or underestimating hidden costs can derail expected returns. Healthcare organizations need expert guidance to navigate compliance, technology selection, and ROI optimization models.
At Emorphis, we have partnered with leading healthcare providers, payers, and innovators to design AI solutions that deliver sustainable ROI. Our expertise covers end-to-end AI software development, integration with EHR systems, regulatory compliance, and performance optimization.
If you are exploring AI adoption in healthcare and want clarity on the ROI models that will work for your organization, we invite you to connect with us.
Contact us today to discuss how we can help you unlock the full economic value of AI in healthcare.